When it comes to treating spinal injuries, percutaneous pedicle screw fixation has emerged as a promising minimally invasive surgical technique. By inserting screws into the pedicles of the vertebral column, this procedure aims to provide stability and support to the spine. While percutaneous pedicle screw fixation offers several advantages, it is essential to consider its pros and cons before determining its suitability for individual cases. In this blog post, we will delve into the world of percutaneous pedicle screw fixation, exploring its benefits and potential considerations.
1. Minimally Invasive Marvels Percutaneous pedicle screw fixation stands out as a minimally invasive approach to spinal stabilization. By utilizing smaller incisions compared to traditional open surgery, this technique offers various advantages. Firstly, the reduced tissue damage minimizes postoperative pain and discomfort, facilitating a smoother recovery process. Patients often experience less pain following percutaneous pedicle screw fixation, allowing for quicker mobilization and improved overall comfort. Additionally, the smaller incisions also contribute to shorter hospital stays, enabling patients to return to their daily routines sooner and reducing healthcare costs.
Furthermore, the minimally invasive nature of percutaneous pedicle screw fixation leads to improved cosmetic outcomes. With smaller incisions, scarring is often less noticeable compared to open surgery, which can be a significant concern for many patients. The enhanced aesthetic results contribute to a higher level of patient satisfaction, boosting self-confidence during the recovery phase.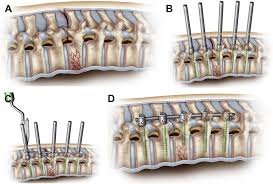
2. Precision Amidst Limitations Although percutaneous pedicle screw fixation offers numerous advantages, it is essential to consider the limitations associated with this technique. One notable limitation lies in the limited surgical exposure it provides. Due to the smaller incisions, the visualization and access to the surgical site may be compromised, making it challenging to address complex spinal injuries or anatomical variations. In cases where extensive exposure is required, open surgery may be a more suitable option.
Another consideration is the risk of radiation exposure. Percutaneous techniques often rely on imaging guidance, such as fluoroscopy, to assist with screw placement. While these imaging techniques are crucial for accurate screw positioning, they expose both the patient and surgical team to ionizing radiation. Repeated procedures or individuals with sensitivity to radiation may necessitate careful evaluation of the risks and benefits associated with percutaneous pedicle screw fixation.
3. Technical Skill: The Key to Success Performing percutaneous pedicle screw fixation requires a high level of technical skill and expertise from the surgeon. Navigating through smaller incisions while accurately inserting screws demands precision and proficiency. Surgeons must undergo specialized training to master the technique and ensure optimal patient outcomes.
The technical complexity of percutaneous pedicle screw fixation is further amplified by the reliance on imaging guidance. Surgeons must interpret real-time imaging data to determine the correct screw trajectory and placement. This necessitates a thorough understanding of spinal anatomy, three-dimensional visualization skills, and the ability to make quick decisions during the procedure. Surgeons who are experienced and well-versed in percutaneous techniques are better equipped to navigate these challenges and deliver successful outcomes.
4. Navigating Neurovascular Risks One potential risk associated with percutaneous pedicle screw fixation is the possibility of neurovascular injury. During the insertion of screws, nearby nerves, blood vessels, or other critical structures may be inadvertently damaged. The close proximity of these vital structures to the pedicles requires utmost precision during the surgical procedure.
To mitigate the risk of neurovascular injury, surgeons employ various strategies. These include preoperative planning using advanced imaging techniques, careful patient positioning, and real-time monitoring of nerve and vessel integrity. The surgical team must exercise caution and expertise to minimize the potential for complications and ensure patient safety.
5. The Fine Balance of Correction Capabilities While percutaneous pedicle screw fixation is effective for stabilizing spinal injuries, its corrective capabilities may have limitations compared to open surgery. Achieving precise spinal alignment and correcting deformities can be more challenging with percutaneous techniques. The restricted visualization and access to the surgical site may impede the surgeon’s ability to make extensive corrections.
However, it is important to note that not all spinal injuries require significant correction or realignment. In cases where the primary goal is stabilization and pain relief, percutaneous pedicle screw fixation may provide sufficient support without the need for extensive correction. The decision between percutaneous and open surgery should be made on a case-by-case basis, considering the specific needs and goals of the patient.
Conclusion: MJ Surgical presents a compelling option for stabilizing spinal injuries, offering advantages such as minimized tissue damage, reduced postoperative pain, shorter hospital stays, improved cosmetic outcomes, and faster recovery times. However, it is crucial to carefully consider the limitations and potential considerations associated with this technique, including limited surgical exposure, radiation exposure, technical complexity, risk of neurovascular injury, and potential limitations in correction capabilities. By weighing the pros and cons in the context of individual patient needs and consulting with skilled medical professionals, informed decisions can be made to ensure the best possible outcomes for spinal injury patients.